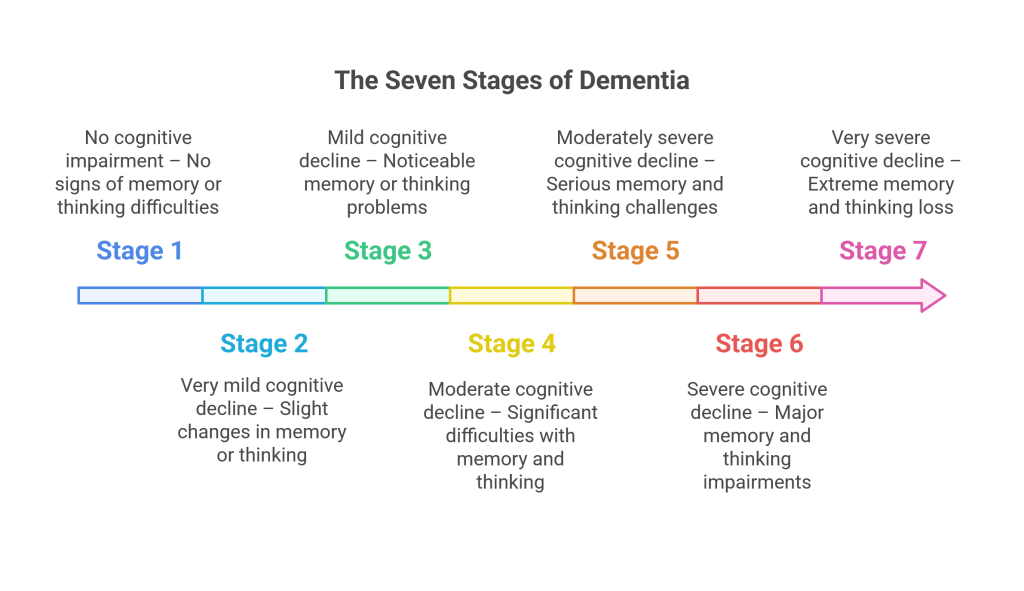
Dementia can bring many changes to an individual. But understanding its stages helps families provide better care with patience and kindness at every step.
While Dementia is an umbrella term with a group of symptoms that affect memory, judgment, and communication, it moves through stages. Some progress slowly through the stages, while others experience changes more quickly. What always matters most is compassion, connection, and understanding. For example, with the Global Deterioration Scale, caregivers can set realistic goals, focus on their strengths, communicate kindly, create moments of joy, and seek support when needed.
In this blog, we’ll walk you through the 7 stages of Dementia in this guide so you have an understanding of the progression of dementia.
What are the 7 Stages of Dementia?
Health professionals use the Global Deterioration Scale (GDS) to analyze the seven stages of dementia. This widely used method helps caregivers and medical experts understand how quickly dementia advances in a patient. It also guides families and caregivers with the symptoms that they must expect among their loved ones at each stage of dementia.
|
Seven Stages of Dementia |
|||
|
Stage |
Cognitive Impairment | Symptoms |
Level of Care Needed |
|
1 |
No cognitive impairment |
Normal function |
None |
|
2 |
Very mild cognitive decline |
Occasional forgetfulness |
Minimal reminders |
|
3 |
Mild cognitive decline |
Noticeable lapses in memory |
Support for organization and planning |
|
4 |
Moderate cognitive decline |
Clear signs of memory loss |
Daily supervision recommended |
|
5 |
Moderately severe decline |
Help needed with daily tasks |
Regular caregiving assistance |
|
6 |
Severe cognitive decline |
Loss of awareness, personality changes |
Full-time caregiving |
|
7 |
Very severe cognitive decline |
Loss of movement, speech, and physical control |
End-of-life and hospice care |
A Quick Look at Different Types of Dementia
|
Type of Dementia |
Typical Progression Pattern |
Key Characteristics |
|
Alzheimer’s Disease |
Gradual decline over the years | Memory loss, confusion, difficulty with words |
| Vascular Dementia | Step-like decline after small strokes |
Sudden drops in function, slowed thinking |
|
Lewy Body Dementia |
Fluctuating symptoms | Hallucinations, sleep issues, movement changes |
| Frontotemporal Dementia (FTD) | Earlier onset (40–65 yrs) |
Personality or language changes |
How Does Dementia Progress?
Dementia typically advances through seven stages, which are grouped into three main phases:
|
Phases of Dementia Progression |
|||
|
Phase |
Included Stages | Level of Independence |
Care Focus |
|
Early / Pre-dementia |
1–3 | Mostly independent | Routine support, memory tracking |
| Middle / Moderate | 4–5 | Partial dependence |
Daily care assistance, safety |
|
Late / Severe |
6–7 | Full dependence |
Comfort, dignity, and end-of-life support |
It’s important to note that the progression of dementia varies for each individual and depends on the specific type, such as Alzheimer’s, vascular dementia, Lewy body dementia, or frontotemporal dementia. Recognizing the signs and symptoms in each phase, particularly the later stages of dementia before death, can help caregivers respond effectively as the condition advances.
Dementia Stage 1: No Cognitive Impairment
Stage 1 of dementia might seem unusual because it typically resembles normal mental function with no noticeable decline. People in the first three stages of dementia usually don’t show enough symptoms for a diagnosis.
Although mild cognitive impairment might exist, stages 1, 2, and 3 on the Global Deterioration Scale (GDS) are considered pre-dementia stages. However, it’s important to understand that changes in the brain are already happening during these early stages, which could progress to a dementia diagnosis by stage 4.
| This stage is often only detected through specialized brain scans or long-term medical observation. |
Dementia Stage 2: Mild Memory Lapses
Stage 2 dementia, also referred to as “very mild cognitive decline,” involves occasional memory slips, such as misplacing keys or forgetting someone’s name. This stage is often considered a pre-dementia phase and does not qualify for an official dementia diagnosis.
Many seniors experience this level of forgetfulness as part of normal aging. The changes are usually so minor that caregivers or healthcare providers may overlook them. Stage 2 is also called “age-associated memory impairment” on the Global Deterioration Scale (GDS). It is a standard part of aging that many older adults face at some point.
According to research by Professor Gary W. Small, published by the British Medical Association, “About 40% of people aged 65 or older have age-associated memory impairment — in the United States, that’s about 16 million people. Only about 1% of them will progress to dementia each year.”
For most people, this pre-dementia phase does not advance to a dementia diagnosis. With healthy lifestyle adjustments supporting brain function, seniors can remain in Stage 2 for a long time or indefinitely.
Stage 2 dementia symptoms include:
- Misplacing familiar items
- Difficulty remembering names of friends, family, or past acquaintances
| About 40% of U.S. adults aged 65 and older, about 16 million people, have age-related memory impairment, and only about 1% develop dementia each year. |
Dementia Stage 3: Mild Cognitive Decline
Stage 3 dementia, often referred to as mild cognitive impairment (MCI) or mild decline, usually does not significantly disrupt daily activities. At this stage, individuals may not yet receive a formal dementia diagnosis, but memory and thinking issues become more apparent to family and caregivers.
How Quickly Does Early Dementia Progress?
According to the National Institute on Aging, around 10–20% of older adults with MCI, aged 65 or above, may develop detectable dementia within a year.
Because MCI can lead to more advanced dementia stages, identifying the signs early and seeking medical advice is vital. Proactive care can help maintain brain health and potentially slow the progression of dementia.
Common signs of this stage include:
- Frequently missing appointments or forgetting events.
- Misplacing items often.
- Getting lost in familiar areas.
- Declining performance at work.
- Struggling to find the right words.
- Repeating statements or questions.
- Difficulty staying organized or focusing.
- Trouble handling complex tasks or solving problems.
- Driving challenges or unsafe driving behaviors.
Recognizing these symptoms early can help families plan for care and better manage the later stages of dementia before death becomes a concern.
Dementia Stage 4: Moderate Cognitive Decline
At stage 4 of dementia, a person shows clear and noticeable signs of mental decline. Their personality may change, and they often display significant dementia-related behaviors. The severe symptoms from stage 3 become more prominent at this stage. Dementia is usually not diagnosed until a person reaches stage 4 or later.
Medically, stage 4 is called “moderate cognitive decline,” but the Global Deterioration Scale (GDS) also classifies it as “mild dementia.” At this point, doctors and caregivers notice clear signs that the Dementia is progressing and requires memory care. These include problems with language and a reduced ability to solve problems.
Symptoms of stage 4 dementia include:
- Withdrawing from social interactions
- Emotional instability or mood swings
- Lack of responsiveness to others
- Decline in intellectual abilities
- Difficulty completing everyday tasks
- Forgetting recent events
- Denying that symptoms are present
If you are in the moderate stage of dementia and want to improve, here are 7 ways to create a daily routine for seniors with dementia.
Dementia Stage 5: Moderately severe cognitive decline
This stage, often referred to as middle-stage dementia or “mid-stage” in the seven stages of dementia, represents a significant shift. At this point, individuals may need help with daily tasks (ADLs), such as dressing and bathing, as well as more complex activities (IADLs), like managing finances or preparing meals.
Stage 5 typically lasts between two to four years, but the progression of dementia varies for each person.
During this phase, your loved one will likely need closer supervision and increased care. While they may still remember important facts about themselves, like their names and children’s names, they might forget details such as their grandchildren’s names, their former addresses, or where they went to high school.
Common Symptoms of Stage 5 Dementia:
- Significant memory loss, including personal details and recent events
- Wandering
- Confusion and forgetfulness
- Disorientation, especially later in the day (sundown syndrome)
- Noticeable decline in mental sharpness and problem-solving skills
Understanding these changes can help you prepare for the stages of dementia before death and provide the support your loved one needs during this challenging time.
| Increased supervision is needed to prevent accidents and ensure safety. |
Dementia Stage 6: Severe Cognitive Decline
Stage 6 of dementia involves a significant cognitive decline, requiring a caregiver to assist with basic daily tasks such as eating, using the bathroom, and personal care. Seniors at this stage may struggle with sleep regulation, interacting with others, and behaving appropriately in public.
As dementia symptoms become more complex in stage 6, you might question whether full-time care is needed. To stay prepared, keep track of symptoms, observe your loved one’s ability to handle daily activities (ADLs) and more complex tasks (IADLs), and consider care options like memory care or home care.
Stage 6 Dementia Symptoms include:
- Difficulty sleeping
- Incontinence (urinary or fecal)
- Aggression and anxiety
- Personality changes, such as paranoia or delusions
- Inability to carry out daily activities (ADLs)
- Severe memory loss
- Inability to recognize family members and caregivers
| It’s time to discuss 24-hour care or memory care facilities for safety and comfort. |
Dementia Stage 7: Severe Cognitive Decline
Stage 7 is the final stage of dementia, often called the end stage. At this point, individuals can no longer care for themselves and become very unresponsive, with both verbal and physical abilities severely declining. Speech is lost, movement is minimal, and essential body functions start to fail.
Symptoms of Stage 7 dementia include:
- Inability to speak.
- Failure to recognize loved ones or caregivers.
- Lack of physical movement without assistance.
- Difficulty chewing or swallowing.
- Impaired bodily functions, including breathing problems and organ failure.
- Excessive sleeping.
- Loss of bladder and bowel control.
This stage marks the final stages of dementia before death, where the person’s health deteriorates rapidly.
| Compassionate end-of-life care, such as hospice or respite support, can ensure dignity and comfort during this stage. |
Managing Behavioral and Emotional Changes in Dementia
Behavior and mood changes can happen at any stage of dementia. Understanding what triggers them helps caregivers handle these moments with patience and care.
Common Behavioral Symptoms of Dementia
- Agitation or anger.
- Hallucinations or delusions. (seeing or believing things that aren’t real)
- Wandering or restlessness.
- Depression, anxiety, or mood swings.
Tips for Managing Difficult Behaviors in Dementia
When you respond calmly and consistently, it helps reduce confusion and fear for the person with dementia.
- Keep a calm, predictable daily routine.
- Use gentle redirection instead of arguing or correcting.
- Surround your loved one with familiar people, objects, and music.
- Avoid overstimulation, keep noise and clutter to a minimum.
Legal and Financial Planning for Dementia Care
Planning ahead makes a big difference in dementia care. Early preparation helps protect your loved one’s wishes and reduces stress later on.
Key Legal and Financial Steps to Take
Early legal and financial planning gives everyone peace of mind and ensures smoother decision-making as dementia progresses.
- Set up a Power of Attorney for health and financial decisions.
- Create advance directives or a living will to outline care preferences.
- Review insurance coverage and options for long-term care.
- Discuss end-of-life preferences openly with family members.
Caring for the Dementia Caregiver
Caring for someone with dementia is deeply rewarding but also physically and emotionally demanding. Caregivers need rest and support, too.
Self-Care Tips for Dementia Caregivers
A healthy caregiver can give better care and stay emotionally balanced.
- Take regular breaks or use respite care services.
- Join local or online support groups for caregivers.
- Keep up with your own doctor visits and health checkups.
- Ask for help from family or professional caregivers when needed.
- Try mindfulness, breathing exercises, or light exercise to manage stress.
End-of-Life and Palliative Care for Dementia Patients
As dementia reaches its final stages, the focus moves from treatment to comfort and dignity. Palliative care helps improve the quality of life for both the person and their family.
Goals of Palliative and Hospice Care in Dementia
Even in the final stage, people with dementia can still feel love and calm through gentle touch, soothing voices, and comforting music.
- Manage pain, breathing, and other physical symptoms.
- Offer emotional and spiritual comfort to the person and family.
- Support decision-making and help families cope with grief.
- Provide round-the-clock hospice care when needed.
Wrapping Up
Understanding the stages of dementia before death can provide important insight into the challenges ahead. As the condition progresses, it’s essential to stay informed and seek support to ensure your loved one’s comfort and well-being.
Whether you’re coping with dementia yourself or caring for a loved one, knowledge is a powerful tool in managing the journey. If you’re considering additional care options, contact communities like Quail Crest for memory care in Eugene Oregon, for compassionate and professional support. Offering services such as hospice respite care can also provide relief for caregivers during this difficult time.